
Plantar Fasciitis - Symptoms and Treatment
By Dawn Morse MSc
As published in International Therapist Magazine
An introduction to Plantar Fasciitis and some techniques to help address the condition:
During the summer months and the road running season, many therapists start to see an increase in injury rates within their clinic. One injury which is often linked to an increase in training load is Plantar Fasciitis.
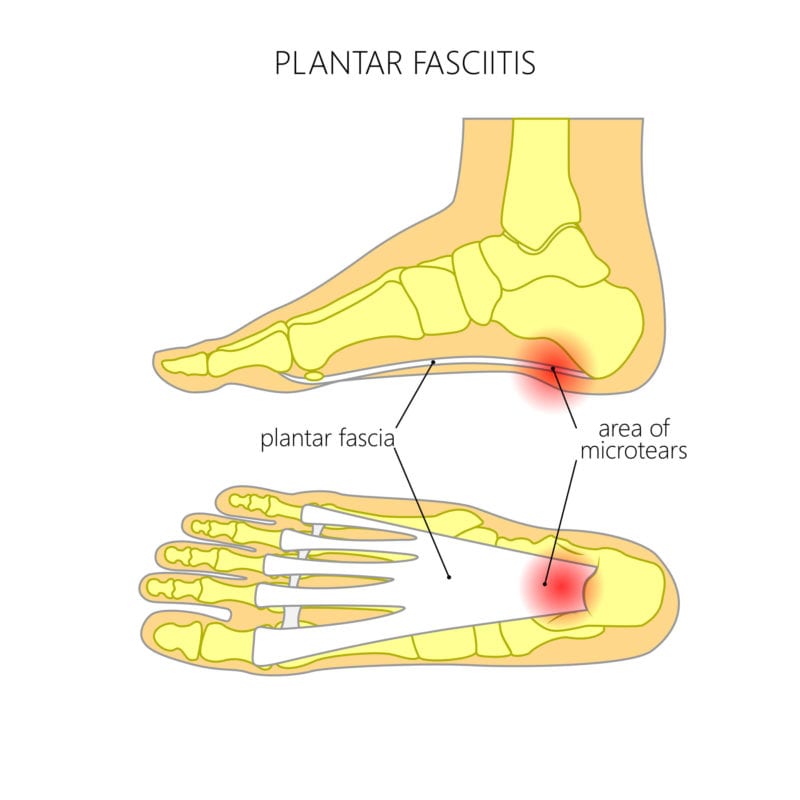
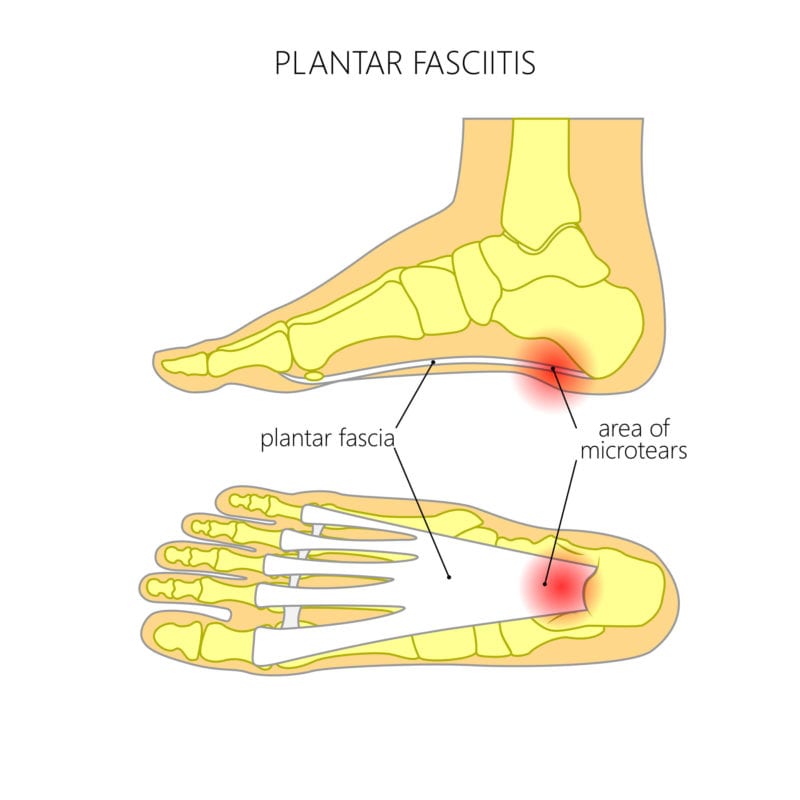
Plantar fasciitis is considered one of the most common causes of heel pain and involves inflammation and sometimes micro-tears, of the plantar fascia, which is a thick band of tissue that runs across the bottom of the foot.
Comon cause of Plantar Fasciitis:
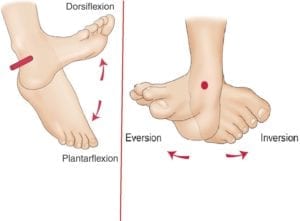
The usual aetiology of this overuse condition is repeated plantar flexion of the ankle, combined with dorsiflexion of the metarsophalangeal joints.
This condition is commonly seen in runners, especially those who have recently started running or who have increased their training load.
It’s also common in dancers and martial artists who often exercise on hard surfaces with little support in footwear, people who are on their feet all day, such as shop workers and nurses; And those who are overweight or have shoes with inadequate support.
Active children can also suffer with this condition, especially if they are playing sports during growth spurts.
Although this is an overuse injury and linked to stress of the plantar fascia, it is linked with tension and shortening of the gastrocnemius and soleus muscles. These muscles form the Achilles tendon, which inserts onto the calcaneus, near to the plantar fascia.
Symptoms:
- Plantar fasciitis typically causes a stabbing pain in the bottom of your foot near the heel.
- Pain is usually worst with the first few steps after waking, and in server cases the foot may not be able to take body weight until the area has been stretched and warmed up.
- Pain may also be triggered by long periods of standing or when getting up after sitting for a long period of time.
- The pain is usually worse after exercise, but often eases during exercise.
- Pain is usually felt on stretching the plantar fascia and tightness is often found in the soleus and gastrocnemius muscles.
- Weakness or tightness may also be found in the tibialis anterior muscle.
- Biomechanical abnormalities may be evident during observation and testing.
Injury assessment:
Palpation, pain questioning, postural observation and walking / running gate are all useful for identifying this condition.
Active, passive and resisted testing should be conducted on plantar flexsion, dorsi flexion, inversion and eversion, along with muscle testing to the gastrocnemius, soleus and tibialis anterior.
The Windlass special test is also useful for confirming tension within the plantar fascia. A positive windlass test will reproduce pain with passive dorsiflexion of the toes.
There are two methods used for conducting the Windlass test, which are essentially weight-bearing and non-weightbearing. The difference between the two is that the sensitivity is increased during the weightbearing assessment. Often testing will start with non-weight bearing, to assess for sensitivity and then move onto weight-bearing testing if required.
Non-weight bearing method (first image below):
Passively raise the toes of the client whilst they are in a seated position to assess for pain.
The client’s knee should be flexed to 90° while in non-bearing position.
The therapist should stabilise the ankle (with one hand placed just behind the first metatarsal head) and extends the metatarsal (MTP) joint.
The test is considered a positive if pain is felt at the end range of the MTP extension.
Weight-bearing position (second image below):
With the client in a weight bearing position, toe extension is created through movement.
Instruct the client to stand on a step and position the metatarsal of heads of the foot to be tested just over the edge of the step.
Instruct the client to place equal weight on both feet.
Then passively extends the first metatarsophalangeal joint.
Passive dorsiflexion of the first MTP joint is continued to its end of range or until pain is reproduced.


Treating Plantar Fasciitis:
Massage techniques
Sports or deep tissue massage can be used to reduce tension in the plantar fascia and associated muscles around the foot and lower leg.
Warming the area with an infra-red lamp or using other heat modalities such as hot stones first may help to reduce superficial tension and enable deeper massage techniques to be more tolerated by the client.
Often massage techniques such as Active Movement, Manual Compressions or Tigger Pointing and Soft Tissue release work well in releasing deeper tension within the soft tissue of the foot and the wider region.
Treatment should be applied to the surrounding muscle groups first, such as the soleus, gastrocnemius, peroneus group and tibialis anterior, to help reduce associated tension in the foot.
Treatment to the plantar fascia itself should be monitored to consider the clients pain levels and to focus on increasing pliability within the tissue.
If manual massage techniques can’t yet be tolerated by the client due to pain levels, Dry Cupping, Dry Needling and Joint Mobilisation techniques can work well to help reduce pain and increase blood flow and mobility.
Some research into the use of therapeutic ultrasound on the plantar fascia, has also shown beneficial results for this condition as the sound waves help to promote blood flow, oxygenation and nutrient levels around the injury site.
When time permits treatment should also include the wider leg such as the quadriceps hamstrings and gluteals, as the client may have been compensating due to pain and walking gate may have been altered, especially in more chronic cases.
Closing the treatment with passive or PNF (proprioceptive neuromuscular facilitation) stretching to the gastrocnemius, soleus and tibialis anterior, can help address muscle memory and function, whilst improving range of motion at the ankle joint.

Rest and active rest
Advising rest from sport or exercise programmes while symptoms cause pain will allow the condition time to heal. However active clients often find rest difficult, therefore active rest can also be advised. This would involve reducing activities that involve the lower limb such as running and cycling and switching to upper body exercise, such as swimming with a float between the legs, using an arm bike or using a rowing machine, but only completing upper body movement.
Self-treatment
To maximise therapy benefits between treatments, the client can use a myofascial release ball or tennis ball to help reduce tension in the foot and to help maintain mobility. If the ball is too intense for the client, then a plastic bottle filled with cold water or ice can be used instead to help roll out the foot.
Stretching:
As Plantar Fasciitis can be linked to reduced flexibility in the lower limb, which limits movement of the foot, stretching should be advised to help maximise treatment effectiveness.
The stretches in Table 1 will help to maintain muscle function and length and reduce muscle tension. While symptoms are present, ideally these stretches should be completed once to twice daily, to aid muscle memory and movement. Each stretch should be held for 15 to 60 seconds.
Table 1: Stretch objectives
| Standing gastrocnemius stretch | To help stretch out the rectus femoris, iliopsoas and the tensor fasciae latae |
| Standing soleus stretch | To help reduce tension in the gluteus maximus |
| Anterior tibialis stretch | To help lengthen the adductor muscle group |
| Plantar fascia stretch | When the condition starts to settle down and is less painful, start to introduce the seated plantar fascia stretch to help lengthen the fascia and to help to maintain blood flow and flexibility |
Hold each stretch for 15 – 60 second and repeat 1 – 3 times when time allows
Gastrocnemius stretch

Soleus Stretch

Tibialis anterior stretch

Stretch to the plantar fascia

When the symptoms of plantar fasciitis start to settle down and is less painful for the client, start to introduce the seated plantar fascia stretch.
Strengthening exercises:
Longer term rehabilitation should aim to develop flexibility around the foot and ankle joint along with foot and calf strength.
When the symptoms have started to settle down foot mobility exercises can be introduced, such as picking up a pencil with the toes, foot writing and calf raises.
Start with completing each exercise once and gradually build up to three sets of each exercise and 5 – 20 repetitions.
Exercises and stretches should be performed on both sides of the body to help maintain function and balance.
Picking up a pencil:
Start by picking up the pencil with the toes 3 to 5 times and then build up to 15 to 20 repetitions.
Writing with the foot:
Start with writing two to three letters and gradually build up to 5 or more words.

Calf raises:
Start with 5 – 15 repetitions on a flat surface and as strength progresses develop the exercise to calf raises from a step, so that the area can be stretched in between each lift.

By Dawn Morse BSc, PGCE, MSc,
Dawn is a sports science and therapy lecturer and the founder and director of Core Elements Training. Core Elements Training offers a range of accredited qualifications and short courses, including Level 3 & 4 Sports and Remedial massage therapy, Level 5 Diploma in Sports and Clinical Therapy and CPD short courses such as Dry Needling, Dry Cupping, Manual Therapy, Electrotherapy and Rehabilitation.


