Weak At The Knees | Core Elements
An introduction to Plantar Fasciitis and some techniques to help address the condition:
The good weather of the summer months and T.V coverage of the London Marathon, Great North Run and the road cycling Tour of Britain and Tour De France, often lead to a up surge of motivation and participation in sports such as running or cycling. Many people are encouraged to take up these sports for the first time in order to get fit or lead a more healthy lifestyle, and recreational athletes are often motivated to start training for a goal of their own, such as their first 10K road run, first half marathon or triathlon etc.
This increase in exercise activity frequently goes hand in hand with an increase in sports related injuries and one of the common injuries seen during this time is Runner’s Knee.
Runners Knee is a term used to describe ilio-tibial band syndrome which is a common condition amongst triathletes, runners and cyclists.
Symptoms and cause of Plantar Fasciitis
This condition usually presents as localised lateral knee pain which is aggravated by activity such as cycling and running downhill.
The pain associated with Iliotibial band syndrome often starts in the same position on the lateral side of the knee. But as the condition worsens through continued training, pain can start earlier and continue for longer after the activity and in some instances, pain can present as far up as the hip or downward towards the fibula or lateral shin region.
Pain and its location is the key symptom of this injury, but in some cases, visible swelling may be present, the area may be tender to touch, and compression and the client may find it painful when walking down stairs. There can be significant tenderness on palpation of the lateral epicondyle of the femur as this condition is caused by excessive friction between the Iliotibial band the lateral epicondyle when the knee is flexed at around 30 degrees.
Swelling in the area may be linked to friction, or injury to the bursa (fluid filled sac) which is located between the Ilio-tibial band and the lateral epicondyle. This bursa is designed to prevent friction, but in the case of this injury the bursa can become impinged or inflamed due to repetitive motion, which leads to additional pain.
Although Ilio-tibial band syndrome is caused through friction, linked to overtraining or excessive overload of training such as, sudden increases in running or cycling distance or an increase in the number of training sessions within a weekly period; this condition can also be linked to exaggerated foot pronation, tibial rotation at the joint and excessive tightness within the Ilio-tibial band.

Injury assessment
Palpation, pain questioning, observation and running gate are all useful for identifying this condition, along with the Obers test.
The Obers test is a Special Test used within examination and assessment of injury, to evaluate a tight, contracted or inflamed Tensor Fasciae Latae (TFL) which runs into the ilio-tibial band. Instead of having its own tendon for muscle attachment, the TFL (along with the Gluteus Maximus) runs into the Ilio-tibial band for insertion to the skeleton.
There are two methods used for conducting the Obers test.

first method
The client is lying close to the edge of the treatment couch with hip and knee flexed in a 90-degree angle.
Therapist stands behind the patient and stabilises the client’s pelvis with one hand.
The other hand holds the medial aspect of the client’s affected knee and places the affected knee in a 5 degree flexion angle, then fully abducts the leg to be tested.
Gravity is then used to adduct the affected leg (without rotating) until the hip cannot adduct any further.
If there is tension within the TFL and associated Iliotibial band the affected leg will stay in an abducted position and will not lower.

second method
The client is positioned on the side of the unaffected leg with the unaffected hip in neutral position and the knee in full extension. The same procedure is then followed.
Once Iliotibial band syndrome has been identified or suspected, treatment should focus on reducing the symptoms such as pain along with the cause, which may be linked to muscle imbalance.
Treating Iliotibial band syndrome
Massage techniques
Sports or deep tissue massage can be used to reduce tension in the associated muscles of the Ilio-tibial band. Massage application and deep tissue techniques such as Soft Tissue Release, Active Movement and Manual Compressions should focus on treating the associated muscle and surrounding area, including the Tensor Fascia Latae, and Gluteus Maximus paying particular attention to the origin and points of interaction with the Ilio-tibial band. Treatment should also cover the quadriceps, adductors and hamstrings muscle groups, along with the gluteus medius and minimus. Dry cupping can be useful for applying to the hamstrings and quadriceps when working on the glutes, as this allows you to be time efficient and can help to reduce pre-tension, when followed up with manual massage techniques.
If treatment time and pain levels allow, massage should also cover the iliotibial band itself with focus to the insertion point to reduce the level of friction being produced around the lateral aspect of the knee.
Closing the treatment with passive or PNF (proprioceptive neuromuscular facilitation) stretching, can help address muscle memory and function, whilst improving range of motion at the hip joint.
Rest and active rest
Advising rest from sport or exercise programmes while symptoms cause pain will allow the condition time to heal. However active clients often find rest difficult, therefore active rest can also be advised. This would involve reducing activities that are hip focused such as running and cycling and switching to upper body exercise, such as swimming with a float between the legs, using an arm bike or using a rowing machine, but only completing upper body movement.
Self-treatment
To maximise therapy benefits between treatments, the client can use a myofascial release ball to help reduce tension in the muscles around the hip. Using the palm, the client can roll the ball with a firm pressure over the muscles at the front of the hip, such as the Tensor Fasciae Latae and quadriceps, to the side of the hip, down the Iliotibial band and over the gluteal muscles.
Stretching
The stretches in Table 1 will help to maintain muscle function and length and reduce muscle tension. While symptoms are present, ideally these stretches should be done two to three times daily, to aid muscle memory and movement. Each stretch should be held for 30 to 60 seconds.
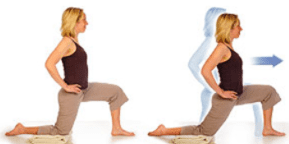
Low lunge with the chest lifted
To help stretch out the rectus femoris, iliopsoas and the tensor fasciae latae.
Tip: hold each stretch for 15 – 45 second and repeat 2 – 3 times when time allows

Lying glute stretch
To help reduce tension in the gluteus maximus

Seated adductor stretch
To help lengthen the adductor muscle group

Piriformis and lateral glute stretch
To help stretch out the external hip rotators.

Hamstring stretch
To help lengthen and reduce tension in the hamstrings muscle group.
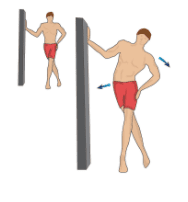
Standing Ilio-tibial band stretch
To stretch out the tensor fasciae latae
Strengthening exercises
Due to the demands of sport and exercise it’s important to stretch and strengthen the associated muscles linked to Ilio-tibial band syndrome. The following exercises can help to address muscle imbalances that may have led to the development of the condition or those that have resulted from the condition itself.
Start with completing each exercise once and gradually build up to three sets of each exercise and 15 – 25 repetitions.
Exercises and stretches should be performed on both sides of the body.
The Clam
Keep your feet together and use your glutes to slowly open and close your legs like a clamshell. Use a smooth controlled motion control and avoid rocking your pelvis during the movement.

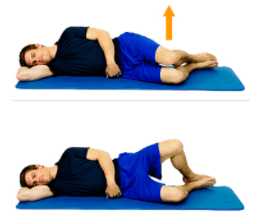
Side leg raise
Using a slow and controlled motion slowly raise your left leg about 45 degrees, then lower.
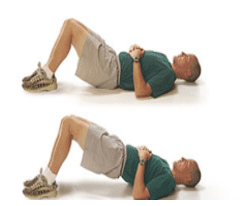
Bridge / Hip Thrust
Press your heels into the ground and use your glutes to raise your pelvis up until your body forms a straight line from your knees to your shoulders.

Side shuffle
Stand with your legs about hip-width apart with an exercise band around your ankles or knees. Take 10 steps to the right and then 10 steps back to the left to complete one set.

Pistol Squat
Stand on your right leg with your left knee raised out in front and slowly lower yourself whilst balancing on the other leg. Lower as far as you can until you gradually reach parallel or 90 degrees at the knee.
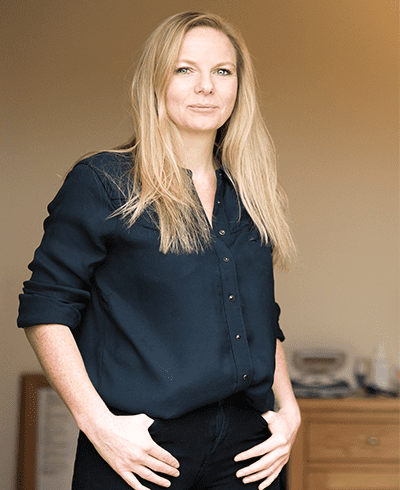
By Dawn Morse, MSc,
Sports science and therapy lecturer and the director of Core Elements Training
Dawn is a sports science and therapy lecturer and the director of Core Elements Training. She offers a range of accredited qualifications and short courses, including Level 3 & 4 Sports and Remedial massage therapy, Level 5 Diploma in Sports and Clinical Therapy and CPD short courses such as Dry Needling, Dry Cupping, Manual Therapy, Electrotherapy and Rehabilitation – www.coreelements.uk.com

